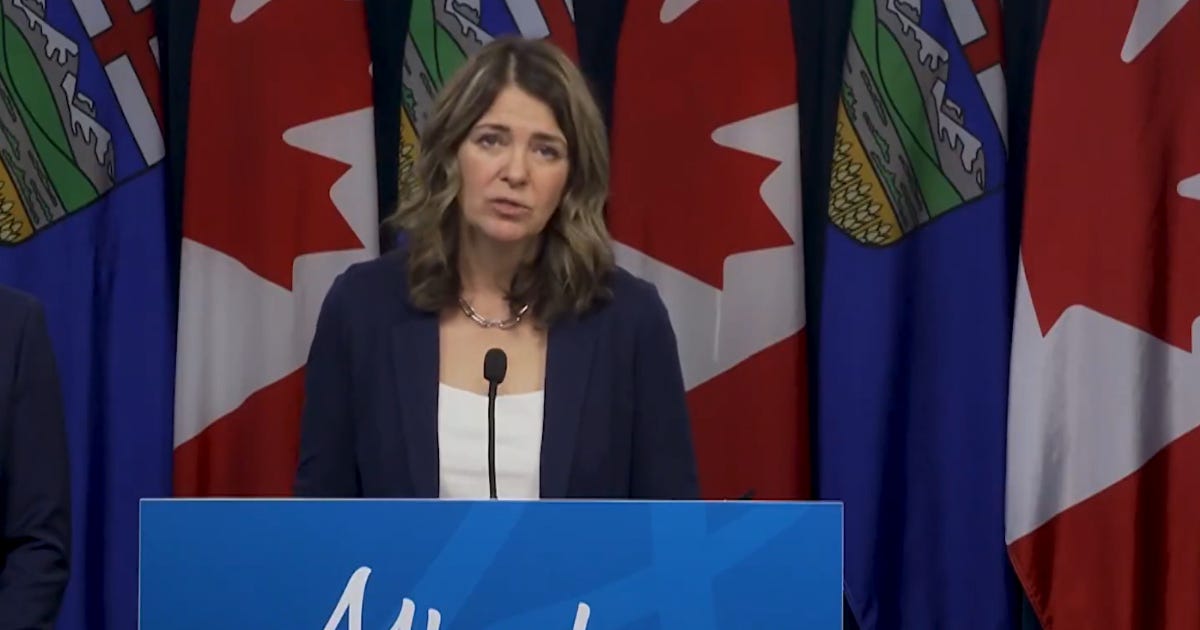
Alberta unveils public-private healthcare model to cut wait times
Alberta’s government is introducing sweeping healthcare reforms that would allow physicians to work in both the public and private systems for the first time under provincial legislation.
Author: Isaac Lamoureux
Alberta’s government is introducing sweeping healthcare reforms that would allow physicians to work in both the public and private systems for the first time under provincial legislation, aiming to expand patient choice and reduce long surgical delays.
Premier Danielle Smith said in a post to X that long delays have left many families waiting in chronic pain.
“Waiting for a needed surgery is a painful and often frustrating experience,” she said.
Bill 11, the Health Statutes Amendment Act, creates a new category of “flexibly-participating” doctors who may choose on a case-by-case basis whether to bill the provincial health plan or charge patients privately. Surgeons could continue to practice exclusively in the public system, exclusively in private settings, or move between both under the new rules.
Smith said the number of people waiting for surgery underscores the need for reform.
“There are now over 80,000 Albertans waiting for elective surgery… and nearly 35,000 of those waiting for these surgeries have been waiting longer than clinically recommended,” she said in the same video.
Under the proposed model, surgeons participating in dual practice could perform publicly funded procedures during daytime hours and then offer private-pay surgeries during evenings, weekends, or at rural sites.
However, the bill includes various provisions to restrict participation. Some include mandating that surgeons in dual practice must perform a dedicated ratio of surgeries in the public system, restricting specialties to public practice if public care would be compromised, and restricting private practice to evenings, weekends, and underutilized rural sites.
Family physicians will not be eligible for dual practice, as the government said in a press conference that family doctors must remain fully focused on public primary care. Emergency surgeries, cancer surgeries and other essential procedures will remain fully public with no private option under any circumstances.
The Alberta government confirmed that its public health guarantee would remain, meaning no Albertan would be forced to pay out of pocket. According to the Alberta government, the changes comply with the Canada Health Act.
Primary and Preventative Health Services Minister Adriana LaGrange said the Canada Health Act “does not preclude private activity,” noting that privately practising physicians already operate in Alberta and other provinces such as Quebec and New Brunswick.
She further told True North that Alberta is continuing to work with the federal government to ensure compliance, noting that Quebec and New Brunswick have not had issues.
In announcing the legislation, Smith stated that the goal is to enhance access to timely procedures while maintaining universal access.
“For years, governments across Canada have tried to fix long wait times by spending more money, yet the problem keeps getting worse. Alberta will not accept the status quo,” she said in the government’s news release.
LaGrange said the reforms are intended to give patients more timely options.
“Albertans are waiting too long for the healthcare they need, so we are taking bold and decisive action to shorten wait times,” said LaGrange.
While the Alberta NDP has framed the change as a move towards “U.S. style healthcare,” LaGrange told True North this is not true, citing European countries and Australia as countries with successful universal healthcare and private systems. She said European systems deliver surgery within weeks or a few months and consistently rank higher in patient satisfaction than those in Alberta.
A Fraser Institute study highlighted the differences between healthcare in Canada and Switzerland, which has integrated private healthcare into its public system. In Switzerland, 85.3 per cent of patients waited less than two months for a specialist appointment in 2022, compared to 48.3 per cent of Canadians.
In Canada, the waiting does not end once an appointment is booked; the median interim period—the time between seeing a specialist and receiving treatment—peaked at 30 weeks last year.
SecondStreet.org recently reported that almost 75,000 Canadians died on surgical and diagnostic wait lists between 2018 and 2024, with tens of thousands more avoiding the system entirely due to delays.
Hospital and Surgical Health Services Minister Matt Jones said the government is also losing surgeons to other jurisdictions and argued dual practice will help retain and attract specialists.
Bill 11 also introduces reforms to drug coverage, billing oversight, food safety standards, and Alberta’s health card system. Private insurance plans would become the first payer for individuals who have them, with public drug programs acting as a safety net.
Assisted Living and Social Services Minister Jason Nixon said the legislation will protect working seniors from losing benefits.
“People shouldn’t be punished for getting older – it’s that straightforward,” Nixon said in the news release.
The bill further repeals the last remaining sections of Alberta’s Hospitals Act, consolidating hospital governance and insurance rules into updated statutes as part of the province’s health system restructuring.


Put a hold on immigration immediately. Our health care system can’t handle an additional million-plus immigrants every year.
There are more people in waiting lines because there are more people sick from vaccines and pharmaceutical drugs